When most people hear the word “amputation,” they immediately think of loss. But for many patients, especially those dealing with severe injury, chronic disease, or cancer, amputation is not about giving up—it’s about survival, relief, and the chance for a better life. Still, it’s not a decision doctors make quickly or easily.
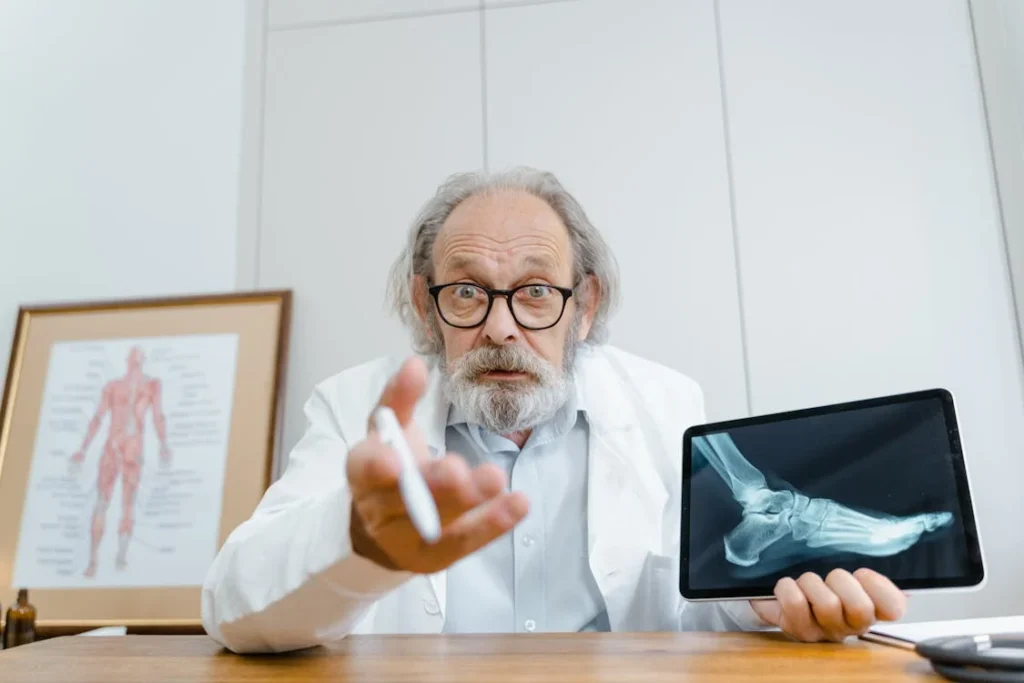
Surgeons take many things into account before they recommend removing a limb. They don’t just look at X-rays or test results. They look at the whole person—their health, their future, and their ability to heal and live well. It’s a serious choice, and it always starts with a deep evaluation of risks, benefits, and possibilities.

When Saving the Limb May No Longer Be Safe
Before a surgeon even begins to consider amputation, they do everything possible to try and save the limb. That’s always the first goal.
Whether it’s a hand, foot, arm, or leg, keeping the natural limb is preferred—if it can be saved safely and if the patient will have good use of it afterward.
But sometimes, keeping the limb can cause more harm than good. Surgeons begin thinking about amputation when the damage is too severe, the risk of infection is too high, or the chance of recovery is too low.
These decisions are rarely made during one meeting. They unfold slowly, over time, as the medical team learns more about the situation.
The Extent of Tissue Damage
One of the first things surgeons look at is how much tissue has been damaged—especially in cases of trauma, like a car accident or industrial injury.
If the skin, muscle, blood vessels, and nerves are crushed or destroyed, it may not be possible to restore proper blood flow and function to that part of the body.
Even if reconstruction is possible, it may involve many surgeries, long hospital stays, and months of rehabilitation.
Surgeons weigh whether the limb, even if saved, would work well enough for the patient to live a full and active life. If not, amputation may provide a quicker, safer path to recovery.
This is not a rushed decision. Surgeons often take time to monitor blood flow, infection, and how the body responds to initial treatment.
But when the chance of saving the limb starts to look slim, the conversation around amputation becomes more serious.
Presence of Severe Infection
Infections that do not respond to antibiotics can become dangerous quickly. Sometimes, especially in cases of diabetes or after a serious injury, an infection spreads deep into the bone or soft tissue.
When this happens, it’s not just about saving the limb—it’s about saving the patient’s life.
Surgeons may try cleaning the wound, removing infected tissue, or giving strong medications. But if the infection keeps returning or threatens to spread to the rest of the body, amputation might be the only way to stop it.
Doctors take into account how long the infection has been present, how deep it has gone, and whether it’s likely to come back.
If there’s a high chance of it spreading into the bloodstream or vital organs, they may recommend amputation as the safest course.
Poor Blood Flow to the Limb
Healthy blood flow is what keeps limbs alive. Without it, tissues can’t heal, fight infection, or stay healthy. Surgeons check for this carefully, especially in people with vascular disease or advanced diabetes.
If blood is not reaching the limb—especially the toes or fingers—the risk of tissue death becomes very high.
Doctors may try to improve circulation through surgery, medication, or lifestyle changes. But if these don’t work, and the tissue continues to die, amputation becomes a way to remove the unhealthy part and prevent future complications.
In some cases, patients may have already lost feeling in the limb. The skin may be turning black or developing sores that don’t heal. These are signs that the tissue is no longer alive—and that the limb may no longer be able to serve its function.

The Patient’s Overall Health and Ability to Heal
A major part of the decision to recommend amputation is the patient’s overall condition. Surgeons don’t look at the limb in isolation—they consider the entire body.
Even if a limb could be saved medically, that doesn’t mean it’s the best option for the patient in the long run.
Chronic Illness and Healing Capacity
People with conditions like diabetes, kidney disease, or heart problems may have a harder time healing after surgery. Their immune systems might be weaker, or their blood flow might already be compromised.
In these situations, limb salvage could lead to longer hospital stays, repeat surgeries, or even life-threatening complications.
Surgeons carefully examine how well a patient’s body can handle a long, complex recovery. If the person is already struggling with other serious health problems, it may be safer to recommend amputation.
While it’s still a major surgery, it can sometimes reduce stress on the body by removing a constant source of pain, infection, or inflammation.
The same thinking applies to people who have undergone chemotherapy or radiation, especially in cancer cases. Their bodies may be tired or fragile, and healing can take longer.
In such cases, doctors might recommend the quicker and more reliable recovery that often comes with amputation and prosthetic use.
Age and Physical Strength
Age on its own doesn’t decide anything, but it does play a role. A younger person with good muscle strength and energy levels might recover better from limb salvage surgery and be more motivated to go through months of physical therapy.
But an older adult with weak muscles, joint pain, or balance issues might have more success using a prosthetic after amputation.
Surgeons think not just about what the limb will look like after surgery—but about how useful and dependable it will be.
If saving the limb means the person still can’t walk well, hold things, or live independently, then they ask whether that surgery is really helping the patient live better.
In these cases, a clean, well-healed amputation can sometimes offer more mobility, less pain, and faster results.
Risk of Repeat Surgeries
Another major concern for surgeons is whether the patient will end up needing several surgeries. Some limb salvage cases are not one-time fixes.
They may involve bone grafts, metal implants, skin flaps, and months of follow-up care. And there’s always a chance that one or more of those steps might fail, leading to infections or implant rejection.
Each surgery takes a toll—physically, emotionally, and financially. If the chance of failure is high, and the likelihood of a useful limb is low, surgeons may decide it’s better to move forward with an amputation early.
This helps the patient avoid extra stress and puts them on a clearer path to recovery and rehabilitation.
Amputation, in such cases, may actually offer a more stable outcome. It’s not without its challenges, but it can reduce the number of future operations and give the patient a chance to rebuild strength and independence sooner.
Functional Outcome: Will the Limb Work After It’s Saved?
Even when it’s medically possible to save a limb, surgeons must ask a difficult question: will that limb be useful to the patient? This is where the idea of functionality comes into the conversation.
Saving a leg that cannot support walking, or an arm that cannot grip or move properly, may not always benefit the patient as much as it seems at first.
Practical Use vs. Emotional Attachment
Understandably, many patients want to keep their limb if possible. The emotional bond is strong—it’s part of their body, their identity.
But surgeons gently help patients see beyond the emotional reaction and think about how the limb will function after surgery.
For example, after severe damage or a tumor removal, the limb might not have the strength or flexibility it once had. A saved leg might still require a brace or a walker.
A saved hand may not regain full grip or sensitivity. If the outcome is a limb that remains painful or difficult to use, it may lower the person’s quality of life over time.
In some cases, patients who choose limb salvage end up needing an amputation later anyway—often after going through multiple surgeries and long recovery periods.
Surgeons aim to avoid this situation when possible, by recommending the clearest and most beneficial path upfront.
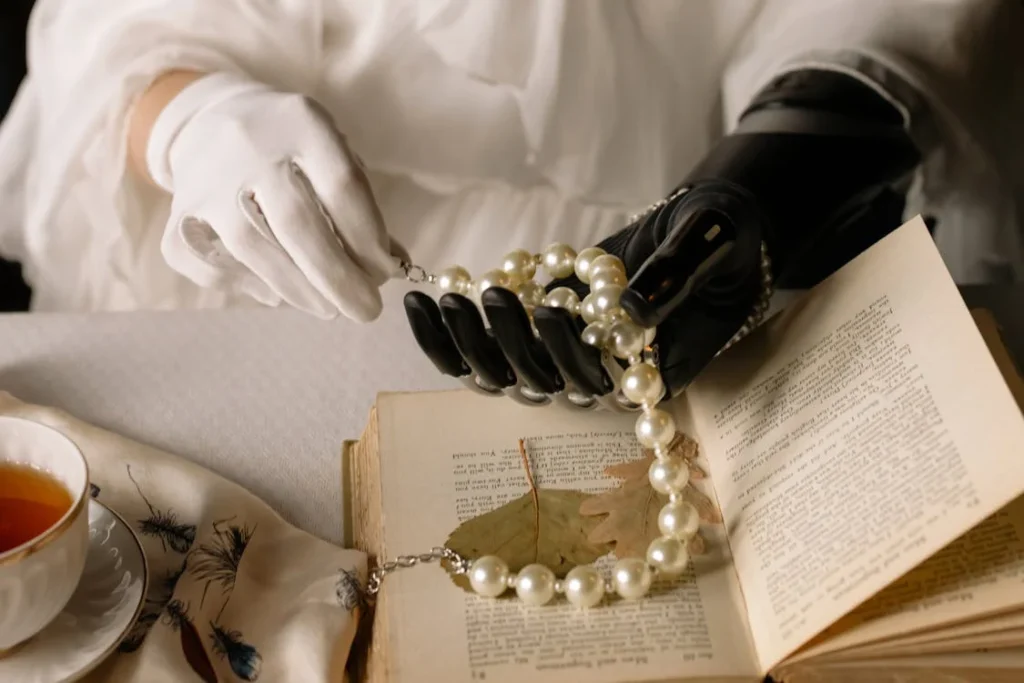
Comparing Outcomes with Prosthetic Use
This is also where prosthetics become part of the conversation. Modern prosthetic limbs, especially when fitted well and supported by rehab, can offer excellent mobility and function.
Some people walk, run, climb stairs, return to work, and take part in hobbies they thought they might lose.
Surgeons consider whether the person might actually do better with a prosthetic, especially if the natural limb is unlikely to provide strong function again.
This isn’t just about physical ability—it’s also about energy, comfort, and independence. A well-functioning prosthetic may allow someone to move with less pain and effort compared to a weak, salvaged limb.
This type of comparison is always handled with care and sensitivity. Surgeons know how personal these decisions are. But at the core, their goal is to help the patient live better—not just to save tissue for the sake of it.

Patient’s Preferences and Lifestyle Goals
A key part of the decision-making process comes from the patient themselves. Every person has different goals, responsibilities, and expectations from life.
Surgeons listen carefully to these points and factor them into their advice. The right medical decision must also align with what matters most to the person.
The Patient’s Voice Matters
Surgeons often begin this conversation by asking what kind of life the patient wants after surgery.
Do they hope to walk again? Go back to work? Care for children? Travel? Continue a physically demanding job? These details are crucial in guiding the decision.
For instance, a patient who works as a manual laborer may need a strong, dependable limb and may not be able to wait for a long recovery after limb salvage. A person who values speed and mobility might find more success with a prosthetic.
On the other hand, a patient with a less physically demanding lifestyle and strong family support may be more open to trying a limb salvage route, even if recovery takes longer.
There’s also the mental and emotional angle. Some patients are very clear that they do not want an amputation unless absolutely necessary.
Others, after understanding the potential outcomes, choose amputation themselves to avoid repeated surgeries and long-term pain.
Doctors do not force the decision. Their role is to guide, explain, and provide honest expectations. The final choice always rests with the patient, and good surgeons respect that.
Cultural and Social Considerations
In India, social and cultural beliefs often influence medical decisions. Some patients may feel pressure from family members or community opinions.
Others may worry about stigma or challenges with marriage, employment, or social status after an amputation.
Surgeons understand that these issues are real and deeply personal. That’s why many now involve counselors, social workers, or even prosthetic experts early in the process—to help patients see what life could look like after either decision.
Involving family members in discussions can also help. When the full picture is shared openly—risks, outcomes, support systems—it becomes easier to make a decision that everyone understands and supports.

Timing and Urgency: When Time Is Not on Your Side
Some decisions can be thought through slowly. Others must be made quickly. Timing plays a big role in whether surgeons recommend amputation.
In many cases, the window for saving a limb is narrow. Waiting too long can lead to complications that make limb salvage impossible.
Trauma and Emergency Situations
In cases of severe accidents—such as road injuries, industrial mishaps, or crush trauma—the decision often comes down to minutes or hours. Surgeons assess the level of damage as fast as possible.
If bones are shattered, skin is torn, and blood supply is cut off, they may need to act quickly.
Even in these situations, doctors try to stabilize the patient first. They check for blood loss, shock, or other injuries. If there’s a chance to save the limb, they may do a temporary fix and reassess.
But if the limb is completely non-viable—meaning the tissues are too damaged to survive—amputation may be necessary right away.
This can be a difficult moment for families, especially if they aren’t prepared. That’s why good trauma surgeons explain everything clearly and support the emotional side of the decision, not just the physical one.
Infection That Won’t Wait
In some cases, infections reach a critical point. The tissue may be turning black, pus may be building up, or the patient may develop a high fever.
These signs indicate that bacteria are spreading fast. If they enter the bloodstream, it could lead to sepsis, which is a life-threatening condition.
When this happens, surgeons can’t afford to wait. If antibiotics don’t stop the infection quickly, and if there’s a high risk to the rest of the body, they will recommend removing the infected part as soon as possible.
This step, though drastic, can save the person’s life.
Patients with diabetes are especially vulnerable. They might not feel pain from a wound until it’s too late.
Regular check-ups and early wound care can help prevent these emergencies, but if it reaches a critical stage, doctors may not have another option.
Advanced Cancer and Fast-Growing Tumors
In oncology, speed also matters. Some bone and soft tissue cancers grow quickly. If they spread into nerves, blood vessels, or nearby organs, removing them becomes more complicated—or even impossible.
Surgeons sometimes recommend amputation early in the treatment plan if the cancer is aggressive and confined to one limb. Doing so can improve survival chances and reduce the need for complex surgeries with uncertain results.
This is not a decision made alone. Oncologists, radiologists, and cancer surgeons work together as a team to review imaging, biopsy results, and treatment responses.
They discuss the pros and cons with the patient and explore whether chemotherapy or radiation could shrink the tumor enough for a limb salvage approach.
When that’s not possible, and if waiting poses too much risk, amputation becomes the safer and more responsible option.
Long-Term Outlook: Thinking Beyond the Surgery
Surgeons don’t just think about what happens in the operating room. They think about what happens in the weeks, months, and years after.
The long-term outcome is just as important as the surgery itself. When making decisions, doctors consider how each path will affect the person’s future.
Quality of Life After Amputation
A well-healed amputation, followed by proper prosthetic fitting and rehabilitation, can lead to a high quality of life. Many people return to work, travel, play sports, and take care of their families.
They learn to move, adapt, and regain their independence.
Doctors take this into account. They consider whether the patient has access to a good prosthetic clinic, rehabilitation support, and follow-up care.
If all of that is in place, and if the limb being saved won’t offer reliable function, amputation may be the better option.
Patients often report reduced pain, easier movement, and fewer complications once they’ve adjusted to their prosthetic. While it does take time and effort, the potential for freedom and confidence is real.
Ongoing Struggles After Limb Salvage
When limb salvage succeeds, it can be incredibly rewarding. Keeping the natural limb can have emotional and psychological benefits. But it often comes with long-term effort—daily therapy, maintenance surgeries, and physical limitations.
Surgeons consider whether the patient will be able to keep up with this journey. They also consider whether the saved limb will bring more benefits or more frustration in the long run.
If the result is a painful, weak, or barely usable limb, then the patient may lose out on quality of life—even though the limb is still there.
By thinking years ahead, not just about the next month, surgeons try to guide patients toward the option that offers not just healing—but living well.

Emotional Considerations and the Role of Support
While surgeons focus heavily on medical and physical factors, they never ignore the emotional side of this decision. Losing a limb—or even thinking about it—can be terrifying.
Patients often experience fear, anger, grief, and confusion. These feelings are normal, and they deserve time and space.
Talking Through the Decision
Surgeons know that recommending amputation is not just a clinical conversation—it’s a personal one. That’s why many hospitals now include counselors, psychologists, or patient navigators in the process.
These professionals help patients and their families understand what to expect, ask questions, and work through their feelings.
In many cases, hearing from others who’ve gone through the same journey makes a big difference. Peer support, survivor stories, and real-world examples help remove some of the fear.
They show that amputation is not the end—it’s a different path, and one that many people walk with strength and confidence.
Surgeons also take time to involve family members. They know that recovery will require support at home, and that everyone needs to be emotionally prepared.
By making space for questions and allowing time to think, they help the patient feel in control of the decision, not pressured by it.
After the Decision: What Comes Next
Once a decision is made, the focus shifts to what comes next—surgery, recovery, and rehabilitation. For patients who undergo amputation, the journey includes wound healing, strength-building, and eventually prosthetic fitting.
For those who choose limb salvage, it may involve follow-up surgeries, braces, or long-term physiotherapy.
In both cases, success comes down to more than just the operation. It depends on care, consistency, and community. A well-supported patient will heal faster, cope better, and move forward with more hope.
At the end of it all, the surgeon’s role is to make sure that every step taken—whether toward limb salvage or amputation—is based on what will give the patient the safest, most functional, and most fulfilling life.
Conclusion
Surgeons never take the decision to recommend amputation lightly. It is one of the most serious, personal, and complex choices in medicine. It involves far more than a medical scan or a test result. It means asking tough questions, considering the whole patient—not just the injured part—and thinking about their future, not just the present.
Whether due to trauma, infection, cancer, or chronic disease, amputation is sometimes the most compassionate and medically sound option. It may offer faster healing, less pain, and better long-term mobility than trying to save a limb that can’t function well again. But it’s always a decision made with care, empathy, and deep respect for the patient’s values and voice.
By understanding what surgeons look for—blood flow, infection risk, function, recovery, long-term use, and emotional readiness—patients can feel more informed and empowered. This knowledge helps make a scary conversation a little less uncertain, and a difficult road a little more manageable.
With the right care, support, and rehabilitation, life after amputation can be full of strength, movement, and purpose. The goal is never just to survive. It’s to heal well, live well, and move forward with confidence.