When someone has a serious injury or illness that affects a limb, they often face a difficult decision—try to save the limb or remove it and move forward with a prosthetic. Doctors, patients, and families all want the same thing: the best possible outcome. But what does that really mean? Does saving the limb always lead to better function? Or can amputation, followed by prosthetic rehabilitation, offer more freedom and strength in the long run?
Understanding Functional Outcomes: What Does It Really Mean?
When people hear the term “functional outcome,” it often sounds technical or hard to relate to. But at its core, it’s quite simple.
It’s about what someone is actually able to do after treatment. How well can they move? Can they return to work? Can they live on their own, take care of themselves, and enjoy life again? These are the real questions behind that phrase.
More Than Just Mobility
Function isn’t just about walking or moving a limb. It includes how well someone can perform basic tasks like standing, lifting, climbing stairs, or holding an object.
It also considers how much energy it takes to do these things. If someone can walk but needs frequent breaks or constant support, their functional outcome is different from someone who walks with ease.
Researchers often look at how far a person can walk in six minutes, how quickly they can get up from a chair, or how steady their balance is. These tests give a glimpse into everyday movement, but numbers don’t always show the full picture.
That’s why it’s also important to consider how people feel about their abilities. Do they feel limited? Are they frustrated or confident? These emotional aspects are part of functional success, too.
Independence and Quality of Life
A strong functional outcome means a person can manage their life without depending on others for everything. They may need some tools or support, but they can get around, care for themselves, and interact with the world in a way that feels natural to them.
Whether it’s returning to work, managing a household, or participating in social activities, these are all signs that someone is functioning well after treatment.
Doctors may also look at the need for long-term support. If a patient requires frequent hospital visits, constant pain medication, or home assistance for many years, that lowers the overall functional outcome.
On the other hand, if they return to work, stay active in their community, and feel mentally strong, it’s considered a good result—even if they have some physical limitations.
How Research Measures Function Over Time
Medical research tries to track these outcomes using simple tools like walking tests, questionnaires, and follow-up visits. One common tool is the SF-36, a survey that asks about physical ability, pain, emotional well-being, and daily function.
Others use scores focused only on limbs, like the LEFS (Lower Extremity Functional Scale).
These tools ask practical questions. Can you walk more than a block? Can you lift groceries? Can you stand for a long time? The goal is to see how much a person’s condition affects their real, everyday activities—not just what the X-rays or scans show.
Researchers often measure function at three key points—short-term (first few months), mid-term (6–12 months), and long-term (1–5 years or more).
This timeline helps show how people recover, how they adapt, and whether one option leads to better outcomes than the other over time.
What Functional Success Looks Like in Real Life
In the end, what matters most is how life feels after treatment. A successful outcome could mean walking without a cane. For someone else, it might mean living without pain or playing with their kids again.
Function is personal. It’s not just about what’s possible on paper—it’s about what’s meaningful to the person living it.
That’s why comparing limb salvage and amputation is complex. One may keep the natural limb but come with lasting pain or weakness. The other may remove the limb but offer smoother recovery, less pain, and quicker return to daily activities with a prosthetic.
Research helps shed light on these differences—but it’s just one part of the picture. The next step is to see what those studies actually say when comparing both paths.

What the Research Says About Limb Salvage Outcomes
Limb salvage is often the first option people consider when a leg or arm is seriously injured or affected by disease. The idea of saving the natural limb feels like the most hopeful path. And in many cases, it can be.
But studies show that the journey after limb salvage isn’t always as simple or successful as people expect. The limb may be saved, but how well it works afterward varies from person to person.
Physical Recovery Is Often Slow and Complex
One of the clearest findings from research is that limb salvage tends to involve longer recovery times. Healing from multiple surgeries, infections, or complications can take many months—or even years.
Some patients report still needing support or therapy well into the second or third year after surgery.
The number of surgeries can also affect function. Studies show that people who undergo repeated operations to fix bone, tissue, or nerve damage often struggle with stiffness, weakness, and long-term discomfort.
These complications can limit how far someone can walk, how much they can carry, or how stable their balance is.
In many cases, even when the limb is technically “saved,” it doesn’t return to full function. It might not support weight well. It may not allow fine movements. For some, it’s painful to use. This can affect how much someone chooses to rely on it—and how much they avoid it entirely.
Ongoing Pain and Medical Dependence
Pain is another major issue reported in limb salvage research. Studies from orthopedic centers and trauma hospitals often note that chronic pain remains a long-term problem for many patients.
This pain may come from damaged nerves, poor blood flow, or muscle weakness that never fully heals.
As a result, some people continue to use pain medication for years. Others rely on braces, crutches, or walking aids. While they may be able to move, the movement often takes extra energy and focus.
This reduces the ease of doing everyday things like climbing stairs, walking long distances, or standing for long periods.
Some research also notes that medical dependence—meaning ongoing hospital visits, physical therapy sessions, and check-ups—remains high for limb salvage patients. This doesn’t just affect the individual. It can place a burden on caregivers, family members, and even finances.
Emotional and Mental Health Challenges
Researchers are also paying more attention to the emotional impact of limb salvage. One key finding is that expectations often don’t match reality.
Many patients go into the process believing their limb will return to normal function. When that doesn’t happen, it can lead to frustration, sadness, or even regret.
Some studies report higher levels of depression and anxiety among limb salvage patients compared to those who chose amputation. This may be linked to the uncertainty of recovery, the slow pace of progress, or the constant medical setbacks.
That said, emotional outcomes vary. Some people feel deeply grateful just to keep their limb, even if it doesn’t work perfectly.
Others say that having the limb—despite the limitations—gives them a sense of wholeness. These emotional values matter too, even if they don’t show up in charts or physical scores.
Returning to Work and Daily Life
Functional return—getting back to work, hobbies, or daily routines—is another area where limb salvage shows mixed results. Some patients do return to their jobs, especially if the job isn’t physically demanding.
But for those in labor-heavy roles, recovery often takes too long or leaves them unable to perform their duties.
Many studies show that return-to-work rates are lower for limb salvage compared to amputation. This isn’t because the limb was saved, but because the function was reduced. Standing all day, lifting weight, or working in fast-paced environments becomes too difficult or painful.
In everyday life, this may also affect how people socialize, travel, or engage in their communities. If mobility is limited or pain is constant, they may avoid outings or activities they once enjoyed.
When Limb Salvage Works Well
Despite the challenges, it’s important to say that limb salvage does work for some people—especially when the damage is less severe or the body responds well to treatment.
A younger, healthier patient with strong support might recover more fully. When the limb heals properly, with fewer complications, function can return close to normal.
Some studies do show decent walking ability and independence among patients who had successful limb salvage. In those cases, the results can be satisfying, especially when the person values having their natural limb over other factors.
Still, research shows that these cases are less common. Most people who choose limb salvage face a longer, more uncertain path—and that’s where it becomes important to compare these results with what’s known about amputation and prosthetic rehabilitation.

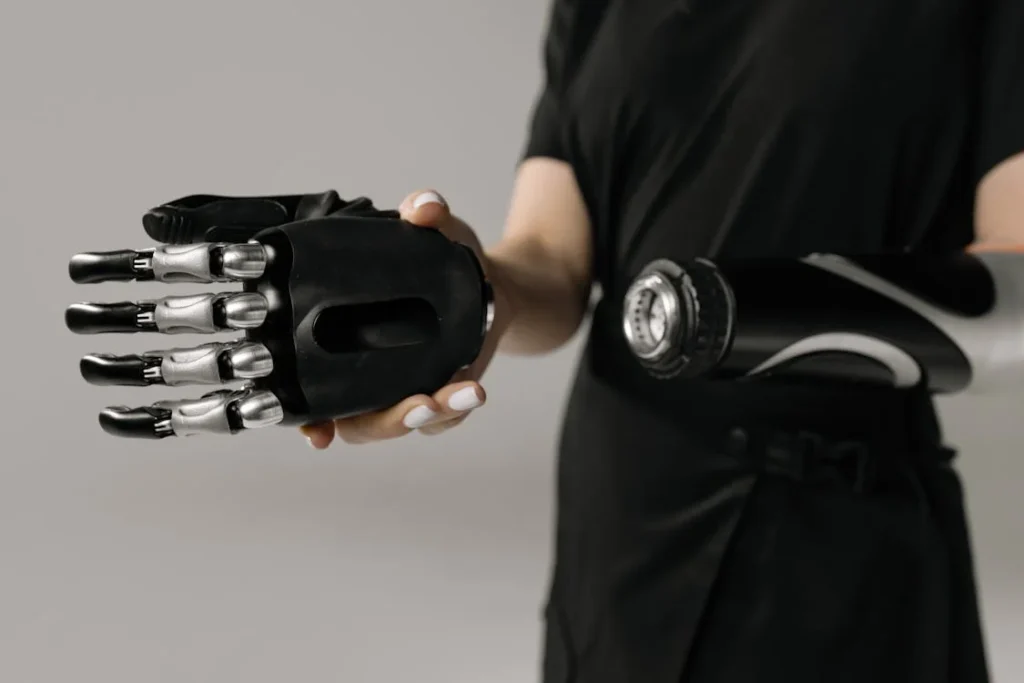
What the Research Says About Amputation and Prosthetic Outcomes
Amputation is a big decision, both physically and emotionally. It often comes with fears—about pain, identity, and the unknown. But once the choice is made, many people discover something surprising: life doesn’t end with amputation.
For a lot of individuals, it actually opens up a clearer and sometimes quicker path to recovery. And research supports that idea, especially when the prosthetic process is well-managed and the user receives the right support.
Recovery Can Be Faster and More Predictable
Unlike limb salvage, which may involve several surgeries and uncertain healing, amputation typically involves a single major surgery, followed by focused rehab.
Once the residual limb heals—usually within a couple of months—patients can begin prosthetic training. That makes the recovery process feel more direct.
Studies from trauma and rehab centers often show that patients with amputations are able to walk again sooner than those who go through limb salvage.
With a prosthetic, many start standing and taking steps within a few months. The timeline is more stable, which helps both the person and their care team plan next steps with confidence.
That consistency also reduces stress. When people know what to expect, they’re better able to stay motivated, follow therapy routines, and move forward. Fewer surgeries also mean fewer hospital stays, less risk of infection, and a shorter interruption to daily life.
Improved Function and Less Pain Over Time
Pain after amputation is real—but for many people, it’s less severe than the ongoing pain that follows limb salvage. Once the surgical wound heals, pain often decreases significantly, especially when the prosthetic fits well and isn’t causing pressure points.
Research has shown that people with well-fitting prosthetics often report lower long-term pain scores than those with salvaged limbs. While some may still experience phantom limb sensations or occasional discomfort, the overall pain burden tends to be lower.
In terms of function, prosthetic users often perform better in daily tasks. Studies comparing walking speed, distance, and balance show that amputees—especially those with below-knee amputations—often score higher than limb salvage patients.
That’s because prosthetic technology has improved dramatically. Lightweight materials, energy-return feet, and myoelectric hands now allow smoother, more natural movement than ever before.
Better Return-to-Work Rates and Independence
One of the strongest findings in research is that amputees are more likely to return to work than those who undergo limb salvage. This is especially true for people who work in physical jobs.
Being able to rely on a prosthetic leg that’s strong, pain-free, and stable allows them to get back on their feet, literally and professionally.
A prosthetic user can often manage stairs, stand for long periods, and lift objects without the same risk of reinjury or chronic pain. This gives them more freedom to take on work responsibilities or pursue education without being held back by their injury.
Daily independence is also higher in many cases. When a prosthetic fits well and is used regularly, people can cook, clean, shop, and travel without needing constant help.
This return to self-reliance builds confidence and improves emotional well-being—something that is deeply valued by users and highlighted often in research.
Emotional Health and Acceptance
Emotionally, the journey after amputation has its own curve. At first, the loss of a limb can feel overwhelming. But what researchers have found is that, over time, many amputees adjust well—and in some cases, better than those who go through limb salvage.
One reason is that the recovery process has clearer milestones. The wound heals, the prosthetic is fitted, and progress can be tracked. This structure gives a sense of control.
In contrast, limb salvage often comes with setbacks—unexpected surgeries, infections, or limited function—that lead to frustration and uncertainty.
Peer support also plays a big role. Talking with others who use prosthetics—through community groups or online forums—helps people share advice, laugh about challenges, and feel less alone. These networks help boost emotional strength and resilience.
Several long-term studies have shown that quality of life scores among amputees often match or exceed those of limb salvage patients.
This doesn’t mean the journey is easy—it just means that, with the right tools and care, life after amputation can be not just manageable, but meaningful and full.
The Power of Good Prosthetic Fit and Follow-Up
One of the key lessons from research is that outcomes after amputation depend heavily on the prosthetic experience. If the socket fits poorly, or if adjustments are delayed, it can lead to discomfort, skin problems, and reduced use.
But with proper fitting, education, and timely follow-ups, those issues can be minimized.
Modern clinics now focus on full-body care—not just the device, but also the training, support, and feedback that make it easier to succeed.
When all these pieces work together, prosthetic users thrive. They feel confident moving, working, and participating in daily life with less pain, less risk, and more independence.

What Head-to-Head Studies Reveal About Limb Salvage vs. Amputation
When someone is faced with the choice between limb salvage and amputation, the hope is that doctors have clear answers about which option leads to better results. But it’s not always that simple.
That’s why researchers across the world have tried to answer this question by comparing both options directly—same types of injuries, similar patient groups, but different treatment paths. These studies give us a deeper, more balanced view of what happens in real life.
Findings From the LEAP Study
One of the most well-known studies in this space is the LEAP study, short for Lower Extremity Assessment Project. It followed hundreds of people in the United States who had suffered severe leg injuries.
Some had their legs salvaged through surgery, while others had amputations and were fitted with prosthetics.
The results showed something surprising. After two years, both groups had similar levels of physical function.
This meant that, on average, those who kept their limb and those who used a prosthetic were doing about the same in terms of walking, working, and handling daily activities.
But the journey to get there looked very different. The limb salvage group often had more surgeries, more hospital stays, and a longer, more painful recovery.
Many faced infections or needed further corrections, which delayed their return to work or full activity. Meanwhile, those who had amputations usually recovered faster and experienced fewer complications overall.
The takeaway wasn’t that one choice is always better—but that amputation, when managed well, can be just as effective as limb salvage, and sometimes easier in terms of recovery.
Quality of Life Measures
Another area where head-to-head studies focus is on quality of life. This includes both physical and emotional well-being, satisfaction with the treatment path, and the ability to do things that matter to the patient.
Several studies from Europe and Asia have found that people who undergo amputation often report higher satisfaction with their decision.
They say that even though losing a limb is hard, they appreciate the stability and predictability of life with a prosthetic. They feel more in control, less tied to hospitals, and more able to plan their future.
People in the limb salvage group, on the other hand, sometimes feel disappointed if the limb does not function as expected.
In cases where pain continues, or movement is limited, it leads to frustration. Some even go on to have an amputation later due to poor function or constant discomfort.
That said, for individuals who do well with limb salvage and have minimal complications, the emotional connection to keeping their limb can be very strong.
They may feel that the effort was worth it—even if the outcome is not perfect. So again, it comes down to how the person feels about their recovery, not just what the medical records show.
Energy Use and Fatigue
A common area of study in head-to-head comparisons is energy use. Researchers have measured how much energy the body needs to perform basic tasks like walking.
It turns out that people with limb salvage often use less energy than above-knee amputees but more than below-knee amputees. This is because salvaged limbs, even when weaker, still offer some natural mechanics that help with movement.
However, this doesn’t always mean they’re more efficient. If walking with a salvaged limb causes pain, uneven steps, or imbalance, the person may tire easily, even if their energy use is technically lower.
Meanwhile, someone with a well-fitted prosthetic may move more comfortably, even if the energy cost is slightly higher.
In real terms, this means that people with prosthetics may be able to walk farther or stay active longer, especially if they’re in good physical shape and their device is well-tuned.
Long-Term Stability and Medical Burden
Another key difference in these studies is how each path affects the person over five, ten, or even twenty years. Limb salvage patients often require more follow-up care. Joint wear, bone fragility, or nerve pain may develop over time. Some need braces or walking aids permanently.
In contrast, people with prosthetics tend to see fewer medical issues once their residual limb heals and they adjust to the device. Repairs and adjustments are part of life, but they are usually manageable and can be done quickly with the right care team.
These differences matter when thinking long term. A younger person choosing between the two might be thinking not just about the next year, but about how their body will feel in twenty years—how it will hold up to work, parenting, or aging.

Key Considerations When Choosing Between Limb Salvage and Amputation
Choosing between limb salvage and amputation is never simple. It’s not just a medical decision—it’s a deeply personal one that affects every part of life, from mobility to emotions to finances.
While research offers valuable insights, the best decision comes from looking at the whole picture, including the person’s health, goals, and lifestyle.
Severity and Type of Injury
The extent of damage plays a major role. If the injury has crushed bones, destroyed nerves, or cut off blood flow, limb salvage may not be realistic or safe.
In these cases, doctors may suggest amputation early on, knowing it offers a clearer path to recovery. On the other hand, if enough of the limb can be saved and restored, and the patient is healthy, salvage might be worth pursuing.
Timing also matters. In emergency cases, quick decisions have to be made. But when there’s time to plan, doctors can perform tests, consult specialists, and weigh the risks of complications more carefully.
Overall Health and Healing Ability
A person’s general health influences how well they recover from either path. Conditions like diabetes, heart disease, or poor circulation can slow healing and raise the risk of infection.
Smokers, for example, often have poorer wound healing outcomes, especially in salvage cases where blood flow is key.
Younger patients may bounce back faster, but even older adults can do well with the right support. What matters most is whether the body can heal and handle the demands of surgery, rehab, and daily use.
Doctors usually take these factors into account when recommending a path. But it’s important for patients and families to understand the risks, so they can plan realistically and avoid surprises later.
Lifestyle, Work, and Daily Needs
What a person wants to return to after recovery is just as important as the medical details. If someone works in a physically demanding job—like construction, farming, or manufacturing—returning with a weak or painful salvaged limb might not be possible.
In those cases, a strong, well-fitted prosthetic may provide more freedom and safety.
The same goes for caregivers or parents. If someone needs to lift children, move around quickly, or handle many responsibilities, they’ll need reliable mobility. A prosthetic might offer that sooner and with more stability than a limb that doesn’t fully recover.
For someone who lives in a multi-story home, travels often, or has limited access to follow-up care, the long-term maintenance of a salvaged limb might be too demanding. These practical details often get overlooked but can greatly affect how someone feels years down the line.
Personal Values and Emotional Readiness
Emotions are part of this decision, and they deserve attention. Some people have a strong desire to keep their limb, even if function might be limited. Others may feel more comfortable moving forward with amputation if it means less pain, fewer surgeries, and faster independence.
It’s also about how someone sees themselves. Body image, cultural beliefs, or personal goals all influence how people view amputation and prosthetics. Talking with a counselor, support group, or others who have gone through the process can help bring clarity.
Emotional readiness matters during recovery too. A person who feels confident and supported is more likely to succeed with therapy, adjust to their device, and stay positive during setbacks.
The choice should reflect what will help them feel whole—not just physically, but mentally and emotionally too.
Access to Care and Follow-Up
The quality of care a person can access—before, during, and after treatment—can affect which option makes more sense. Limb salvage often requires specialized surgical teams, regular therapy, and close monitoring. If those services aren’t easily available, recovery becomes harder.
Prosthetic care also requires skilled fitting, adjustments, and training. But once the device is in place and the user is confident, fewer visits are usually needed over time.
In India, where rural areas may lack high-level surgical support, a good prosthetic solution may offer better outcomes simply because follow-up care is more accessible. This makes local support networks, rehab programs, and repair services an important part of the decision process.

Cultural Perceptions and Social Influences on Recovery
The journey of recovery after limb salvage or amputation is shaped not only by physical and emotional factors, but also by the environment in which a person lives.
Culture, society, and even public attitudes play a large role in how people view their options—and how they feel about their bodies afterward. In many cases, these unseen influences affect the success of recovery just as much as the treatment path itself.
Social Stigma and Body Image
In many parts of the world, including India, the idea of living with a visible limb difference or prosthetic can carry social weight. Some people worry about how they will be seen—by their community, their workplace, or even their own family.
This can lead to pressure to preserve the natural limb at all costs, even if it means living with pain or poor function.
Limb salvage may be viewed more positively in some social settings because it appears to maintain physical “wholeness.” But what’s not always understood is that the function of that limb may be severely reduced.
In some cases, people who choose salvage later feel frustrated if the limb doesn’t allow them to live independently or return to their normal routine.
Meanwhile, those who undergo amputation and use a prosthetic may face questions or assumptions about their abilities.
These reactions, while often unspoken, can create a mental hurdle that affects confidence and self-image. How society responds can either support or delay emotional recovery.
These concerns are very real, especially for younger individuals, women, or those in professions where appearance plays a larger role. Understanding and openly addressing these feelings can make a big difference in how someone adjusts.
The Role of Family and Community
Family often plays a major role in medical decisions, especially in collectivist cultures where care is shared and recovery is a group effort. In such settings, the opinions of parents, spouses, or elders can strongly influence whether someone chooses limb salvage or amputation.
In many families, there’s a deep emotional desire to avoid amputation, even when medical advice leans toward it. This can lead to long discussions, delayed decisions, or pressure to try every possible treatment before considering prosthetic rehabilitation.
At the same time, strong family support can be a huge advantage. When families offer encouragement, attend rehab sessions, or help manage therapy routines, outcomes improve—regardless of which path is chosen.
Community support also matters. People are more likely to recover well if they feel accepted, included, and supported in social settings. When others treat prosthetic users with respect and ease, it helps reduce shame or hesitation.
On the other hand, if they face pity or awkwardness, it can create emotional setbacks that slow progress.
Changing the Conversation Around Disability
Another important factor is how disability itself is seen within a culture. If disability is viewed with fear, silence, or discomfort, individuals may hide their prosthetic or avoid public spaces altogether. This limits their activity and makes it harder to return to normal life.
But if disability is framed as a difference—not a weakness—then people feel more confident engaging with the world. They take ownership of their journey, speak openly about their experiences, and even inspire others.
Fortunately, the cultural narrative is beginning to shift. More media coverage, visibility of successful prosthetic users, and public campaigns have helped normalize limb difference and challenge outdated beliefs.
Schools, workplaces, and health organizations are gradually becoming more inclusive, creating an environment where people feel safe to be themselves.
This shift also helps patients make clearer choices. When amputation is no longer seen as a tragedy, but as a viable, empowered medical decision, more people feel comfortable choosing it—especially when it offers better function and independence.
Local Beliefs Around Healing and Technology
In some communities, there is a strong belief in natural healing. People may trust traditional medicine more than surgical solutions. In these cases, limb salvage may feel more “aligned” with local customs, while prosthetics, being mechanical, may feel foreign or overly modern.
Others may see technology as a symbol of progress and independence. In cities and more urban spaces, prosthetic users often report positive reactions and curiosity about their devices. This makes it easier to wear them openly and take pride in recovery.
How technology is viewed—either as helpful or intrusive—can affect how easily someone adapts to a prosthetic and whether they seek upgrades, repairs, or follow-up care when needed.
Conclusion
Choosing between limb salvage and amputation is never just a medical decision. It’s a personal journey shaped by physical recovery, emotional readiness, cultural beliefs, and life goals. Research shows that both options can lead to meaningful outcomes, but the paths look very different. Limb salvage may preserve the limb but often brings a longer, more uncertain recovery. Amputation, followed by prosthetic rehabilitation, can offer quicker function and stability, especially with the right support and care.
What matters most is that the decision reflects the person’s needs—not just in the hospital, but in everyday life. Whether someone chooses to save their limb or move forward with a prosthetic, the focus should always be on helping them live well, feel confident, and return to the life they want.
The best outcomes happen when patients are informed, supported, and empowered to choose what’s right for them—not what’s expected. With continued advances in care and changing attitudes in society, both paths can lead to strength, independence, and a future full of possibility.